Communicating at admission
Effective communication and coordination of care is essential across all points of care
Admission refers to the processes, tools and techniques by which an episode of care is formally commenced by a health professional or health service organisation involving their acceptance of responsibility for a patient and/or their treatment and care.
Key messages
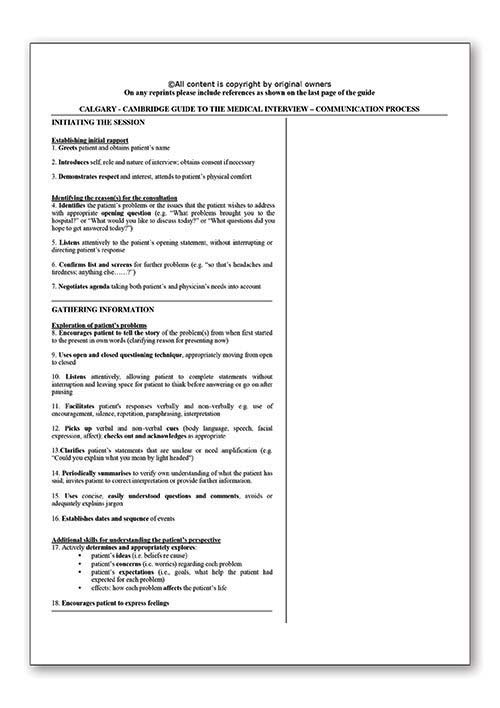
Communication skills
Communicating effectively with other members of the care team and teamwork
- Undertaking structured communication
- Using agreed and common language
- Using ‘check-back’ - a strategy that ensures messages and information are received
- Having situational awareness
- Documenting essential information.
Communicating effectively with patients, families and carers
- Building relationship
- Listening respectfully
- Providing structure
- Initiating the session
- Gathering information
- Explanation and planning (includes risk communication and shared decision making)
- Closing the session.
For more information see Communicating with patients and colleagues
Communication strategies
Why is this important?
Poor communication and information collection at the time of admission increases the risk of harm to patients and can contribute to subsequent errors that will impact on the safety and quality of patient care.
Effective communication with patients, carers and families during the admission process is essential to ensure clinicians have all the relevant information (history) to undertake high-quality clinical assessments, make accurate diagnoses and safe decisions about care. Collecting an incomplete history or story from the patient, family or carer can lead to incomplete information being relied on and delays in appropriate treatment.
When a patient experiences multiple admissions (or readmissions), it is particularly important to ensure that the information available is accurate, complete and up to date (this includes details about previous admissions). This is intrinsically linked with transfer, referral and discharge processes and how information is communicated and integrated across these points of care.
Effective communication with patient, families and carers is also important to ensure patients understand and are involved in any decisions about their care going forward and that there is informed consent.