Communicating to plan care and when providing care
Effective communication is crucial in planning and providing care that is aligned with the patient’s goals of care and health care needs, considers the effect of the patient’s health issues on their life and wellbeing, and is clinically appropriate. When clinicians work in partnership with patients and communicate well with other members of the healthcare team, individualised comprehensive care can be delivered that includes strategies to prevent and manage the risks of harm.
Key messages
Communicating to plan care
- Patients have a key role in planning their care
- Effective communication with patients, families and carers is essential to ensure that decisions about treatment and care are shared, clinically appropriate, and reflect the patient’s preferences and goals
- It is important to tailor communications to patients, families and carers health literacy needs and to consider cultural and linguistic factors. This includes considering if an interpreter is needed
- Effective communication between all members of the care team (across disciplines) ensures there is comprehensive care planning and that the care plan reflects the agreed shared goals for care
- Comprehensive care planning includes a shared understanding of roles and responsibilities for patient care
- Documentation of the agreed care plan is essential to support the delivery of safe patient care.
Communicating when providing care
- Effective communication with the patient when providing care, therapy or medication is important to ensure that the right care or treatment is provided, to treat patients with dignity and respect through keeping patients informed about and involved in their care, and to check a patient’s understanding of any information provided
- Communicating with and engaging a patient in their care provides an opportunity for them to partner in their care to the extent that they choose. This contributes to improved patient outcomes
- To deliver comprehensive care, members of the care team need to effectively communicate and collaborate with each other.
Communication strategies
Shared decision making is more than just building rapport and having a discussion. It is an iterative process of bringing the best available evidence into the consultation, and incorporating it into a discussion that considers the patient’s values and preferences. It can be thought of as the integration of communication and evidence skills to come to a shared decision about what is optimal care. Shared decision making involves explaining:
- Each treatment option
- The quantitative evidence of the risks and benefits of each option
- Then exploring with the patient their preferences and what matters to them.
Guides and tools
Patient-clinician communication - information sheets, posters and research
Health literacy resources
- Shared decision making resources
- Shared decision making an overview (video 1:48)
- Shared decision making challenging myths (video 1:52)
- Shared decision making patient decision aids (video 3:34)
Further reading
- Shared Decision Making webinars - Centre for Medical Psychology and Evidence-Based Decision Making (CeMPED) symposium
- Health Literacy: Taking action to improve safety and quality (96 pages)
- Implement Teamwork and Communication – resources from the CUSP toolkit – AHRQ (US Agency for Healthcare Research and Quality)
Decision support tools can be electronic or paper-based resources that support shared decision making by helping consumers and clinicians draw on high-quality information about particular conditions; compare benefits and harms of each option; and clarify consumers’ values about what matters most to them.
A type of decision support tool are patient decision aids, and it has been shown that people who have used patient decision aids feel more knowledgeable, better informed and clearer about their values. When clinicians use decision support tools to complement their communication skills, patients are actively involved in decision making and have more accurate perceptions about risk.
Guides and tools
Patient decision aids – information and resources
Shared decision making patient decision aids (video 3:34)
- Shared decision making resources
- Ask Share Know – information to assist making medical decisions about your care with health professionals
Further reading
- Shared Decision Making webinars - Centre for Medical Psychology and Evidence-Based Decision Making (CeMPED) symposium
- Engaging patients and their families in their healthcare – resources for different care settings - AHRQ (US Agency for Healthcare Research and Quality)
Clinicians need to work together and collaboratively with patients, using shared decision making and goal-setting processes, to develop care plans that direct the delivery of safe and effective care. Screening, assessment and identification of risks provide a foundation for planning comprehensive care that meets patient needs.
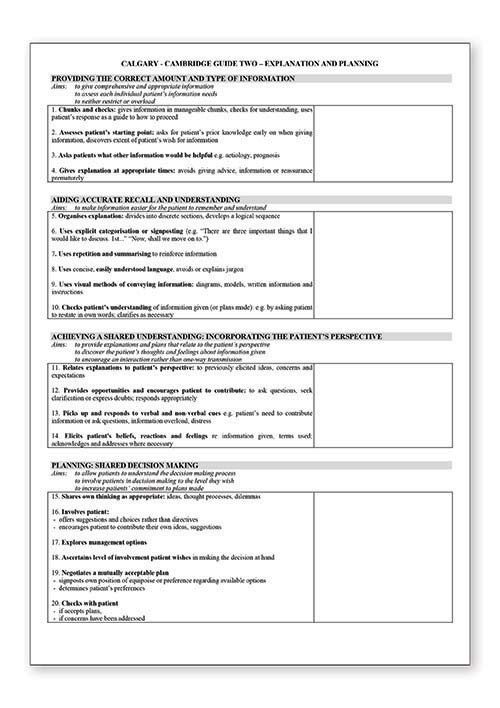
It is necessary for clinicians to refine their skills and capacity to provide person-centred care when developing individualised care plans. Dimensions to consider when explaining and planning care include:
- Respect for patients’ preferences and values
- Emotional support
- Physical comfort
- Information, communication and education
- Continuity and transition
- Coordination of care
- The involvement of family and friends
- Access to care
Guides and tools
Patient-clinician communication - information sheets, posters and research
- Assessing the need for an interpreter (Centre for Culture, Ethnicity and Health)
- Shared decision making resources
- Health Translations Directory - resources for healthcare providers working with patients from culturally and linguistically diverse communities - Victorian Government
- Teach-back interventions - AHRQ (US Agency for Healthcare Research and Quality)
- Using teach-back via an interpreter (Centre for Culture, Ethnicity and Health)
Further reading
- Shared Decision Making webinars - Centre for Medical Psychology and Evidence-Based Decision Making (CeMPED) symposium
- Engaging patients and their families in their healthcare – resources for different care settings - AHRQ (US Agency for Healthcare Research and Quality)
Communication breakdown is a well-recognised contributor to adverse patient outcomes. Effective communication is imperative for good team work, and team work is essential to patient safety. Using structured communication techniques can improve the transfer of clinical information and responsibility between clinicians, and strengthen teamwork behaviours and attitudes.
Effective teamwork enhances patient outcomes and satisfaction, reduces adverse events and has positive organisational benefits such as reduced lengths of stay and hospitalisation costs. The advantages to individual team members include role definition and clarity, stronger work relationships, better accessibility to patients and increased job satisfaction and wellbeing.
Guides and tools
ISBAR app for IOS devices – NSW Health
ISBAR: Identifying and Solving Barriers to Effective Handover in Inter-Hospital Transfer - Case Study 2 (4:02) video
- TeamSTEPPS® resources - SA Health
- Team Stripes - a framework used to enhance teamwork and communication for clinicians working at the point of care - Clinical Excellence Commission NSW
Also see:
- How to communicate within a team - under Communicating with patients and colleagues
- Implementation Toolkit for Clinical Handover Improvement- under Simple Solution development
Further reading
- TeamSTEPPS Implementation of a teamwork programme into an Australian setting: Public report on pilot study (21 pages)
- Core CUSP (Comprehensive Unit-based Safety Program) Toolkit – training resources and tools to improve teamwork to build capacity to address safety issues - AHRQ (US Agency for Healthcare Research and Quality)
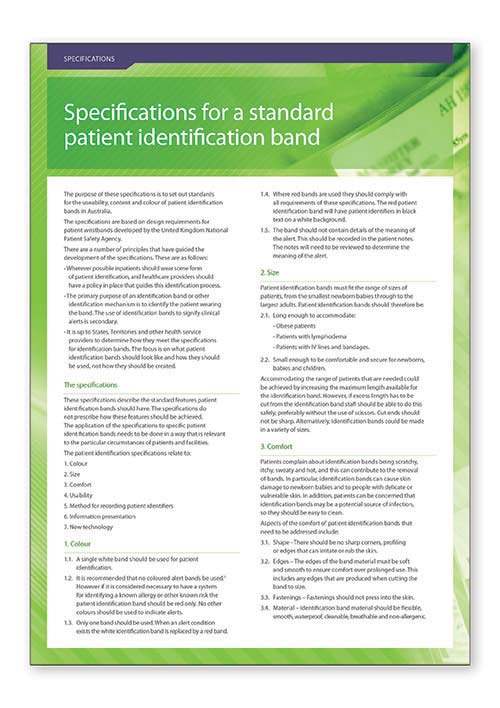
Ensuring the right care is given to the right patient is an essential part of safe care. Patient identification is an activity that is performed routinely in all care settings and can often been seen as a relatively unimportant task. However, it is vital that safety processes are adopted for common tasks to prevent simple mistakes that can lead to patient harm.
Health service organisations are required to implement processes that define approved identifiers for patients. Clinicians must be familiar with their organisational process and use three approved identifiers on registration and admission; when care, medication, therapy and other services are provided; and when clinical handover, transfer or discharge documentation is generated.
Guides and tools
Also see:
Mismatches between patients and their care can have significant consequences including death or major permanent loss of function. While not always resulting in harm, failure to correctly identify patients and match that information to an intended treatment or intervention may result in procedures being performed on the wrong person, wrong side or wrong site; medication errors; blood transfusion errors; and errors in diagnostic testing.
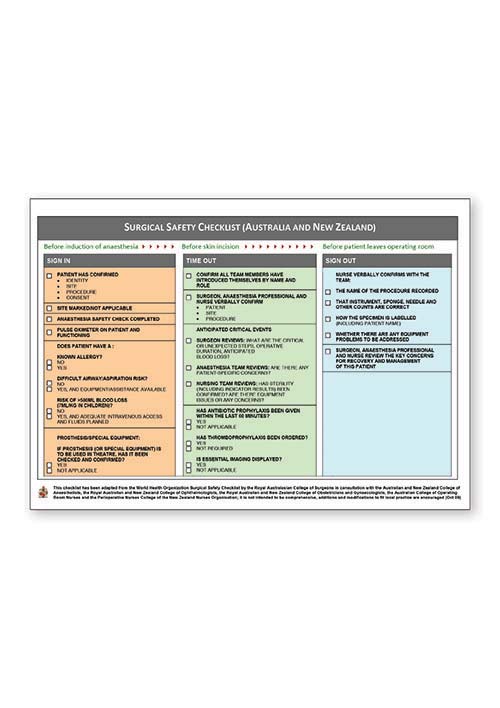
Clinicians must be familiar with their organisational processes for matching patients to their care. The diligent use of checklists and tools to correctly identify patients and match them with their intended treatment helps prevent errors from occurring.
Guides and tools
Surgical Safety Checklist (Australian and New Zealand edition)
Correct Patient, Correct Site, Correct Procedure protocols and factsheets
Also see:
- Correct patient correct site correct procedure checklist - RACGP
- Surgical Team Safety Checklist - South Australia Department of Health resources
Why is it important?
A significant proportion of potentially preventable adverse events are underpinned by failures in communication and team work. Safe, continuous and coordinated care relies on clinicians to partner with their patients, and work together as a team to achieve shared goals and outcomes for patient care.
Essential to this is the need for effective communication and collaboration, between individual clinicians and other members of the healthcare workforce (including managers and administrative staff); across multidisciplinary teams and services; and between healthcare providers and patients, their families and carers.
Taking action: What is my role?
As a leader in your organisation, you have a responsibility to ensure that the systems and processes in your organisation support clinicians to effectively communicate with patients, families, carers and other members of the care team when planning care and delivering care.
Effective communication is a key requirement of the NSQHS Standards (second edition). The following table describes actions in the NSQHS Standard (second edition) that are relevant when communicating to plan care, or communicating when care, treatment or medication is provided.
| Action | Description |
|---|---|
| 2.6, 2.7 | Sharing decisions and planning care |
| 2.8, 2.9, 2.10 | Communication that supports effective partnerships |
| 4.11 | Provide patients with information on their individual medicine needs and risks |
| 5.4-5.36 | Develop, document and communicate comprehensive care plan, provide care to patients in setting that best meets their clinical needs, ensure timely and appropriate referral and identify clinician with overall accountability for a patient’s care |
| 5.5, 5.6 | Multidisciplinary collaboration and teamwork |
| 5.13, 5.14 | Develop and use the comprehensive care plan |
| 5.15, 5.17, 5.19, 5.20 | Provide comprehensive care at the end of life |
| 5.29, 5.30 | Provide care to patients who have cognitive impairment or are at risk of delirium, collaborate with patients, carers and families and manage the use of antipsychotics and other psychoactive medicines |
| 6.5, 6.6 | Correct identification and procedure matching |
| 6.11 | Documentation of essential information in the healthcare record |
For more information see NSQHS Standards (2nd ed.)
You have a key role and responsibility to effectively communicate with your patient and other members of the care team when you are planning and delivering care.
This requires an understanding of health literacy and communication skills in ensuring two-way (or multi-way) communication, building rapport and trust, and managing and communicating risk. Clinical decisions should be made with the patient to incorporate their values, goals and concerns, and considering the best available evidence about benefits, risks and uncertainties of treatment.
Effective communication and collaboration with patients, families, carers and other clinicians involved in care ensures that the care you provide is safe, appropriate, coordinated and meets the goals and preferences of your patient.
- Engage with your clinicians and discuss your goals of care, expectations, and preferences including if you have an advance care plan
- Involve family members, carers or advocate in communication and decisions about your care
- Ask for help if you need a support person, an interpreter or other help to communicate
- Be open, honest and communicate any changes about your medical history, medicines and your health including if your family or carer notice a change in your condition
- Ask questions and raise any concerns you have about your care
- Provide feedback throughout your care experience
- Discuss your ongoing care needs and plan for when you leave hospital. Ask about follow-up appointments and any instruction to optimise your recovery, involve your family or carer, and if not provided, ask for a copy of your discharge summary.
- Australian Charter of Healthcare Rights (2nd edition) and supportive resources
- Communicating with your healthcare provider factsheet
- Communicating with your healthcare provider when you are in hospital posters
- Top Tips for Safe Health Care - includes translations in 15 languages
- Patient decision aids
- NPS Medicinewise Consumer Information
- NPS Medicinewise Medicine Finder - downloadable consumer medicine information sheets
- Choosing Wisely - Resources to reduce unnecessary tests, treatments and procedures
- Ask Share Know. Helping people to get the information that they need and to share in making medical decisions about their care with health professionals
- Question Builder – tool for preparing for your medical appointment by creating a list of questions to ask your doctor - Health Direct
- Decision aids: how they can benefit you infographic
- Sore throat: should I take antibiotics? - decision aid
- Acute bronchitis: should I take antibiotics? - decision aid
- Middle ear infection: should my child take antibiotics? – decision aid
- Communicating in hospital – consumer resource about communication in hospitals – Victoria State Government Health and Human Services