Documentation is an essential component of effective healthcare communication. Given the complexity of healthcare and the fluidity of clinical teams, healthcare records are one of the most important information sources available to clinicians. Good documentation contributes to better patient outcomes by enabling information exchange and continuity of care by all members of the healthcare team.
Key messages
What are the different types of clinical documents in health care?
Clinical documentation is information that is recorded about a person’s care. The primary purpose of clinical documentation is to facilitate safe, high-quality and continuous care.
Clinical documents can take on a number of forms and be paper-based, electronic or a mix of both. These documents include treatment and observation notes, care plans, correspondence, test results, x-rays, clinical photos, medication charts, checklists, operation reports, transfer forms, clinical summaries and information from specialists, community workers or general practitioners.
The healthcare record
The primary place for clinical information to be documented is in the healthcare record. The healthcare record can be made up of a number of different clinical documents, and is the place in which all relevant clinical information about a patient is stored. This includes information about the patient’s medical and social history, about the progress and health outcomes of each intervention or interaction, and information from families and carers.
Documentation needs to be an accurate reflection of clinical events and clinician decision making for classification (coding) purposes as well as a method of communication to facilitate continuity of care. Clinical coding is a health administration function that abstracts clinical information from the healthcare record for the assignment of standardised ICD-10-AM (International Statistical Classification of Diseases and Related Health Problems) and ACHI (Australian Classification of Health Intervention) codes.
Accurate documentation of diagnoses and patient care interventions ensures correct translation of data and appropriate coding. Clinical coding data is used for health resource planning and allocation, epidemiological studies, clinical benchmarking, and financial reimbursement determined on casemix based payments.
Other documents that support safe transitions of care
Transitions of care are high-risk situations for patient safety. It can be common for patients to experience multiple transitions of care when they go through the health system.
Documentation is a way in which the reliability of information is maintained, and shared between different treating clinicians and with the patient, their family or carer. High-quality documentation of clinical information is therefore essential to ensure that clinicians have available all of the information they need to safely transfer the care of a patient.
Clinical documents that support safe transitions include care plans, transfer, referral and request forms, event summaries, short stay summaries, discharge summaries and shared health summaries. These documents have a specific purpose and aim to facilitate the continuity of care.
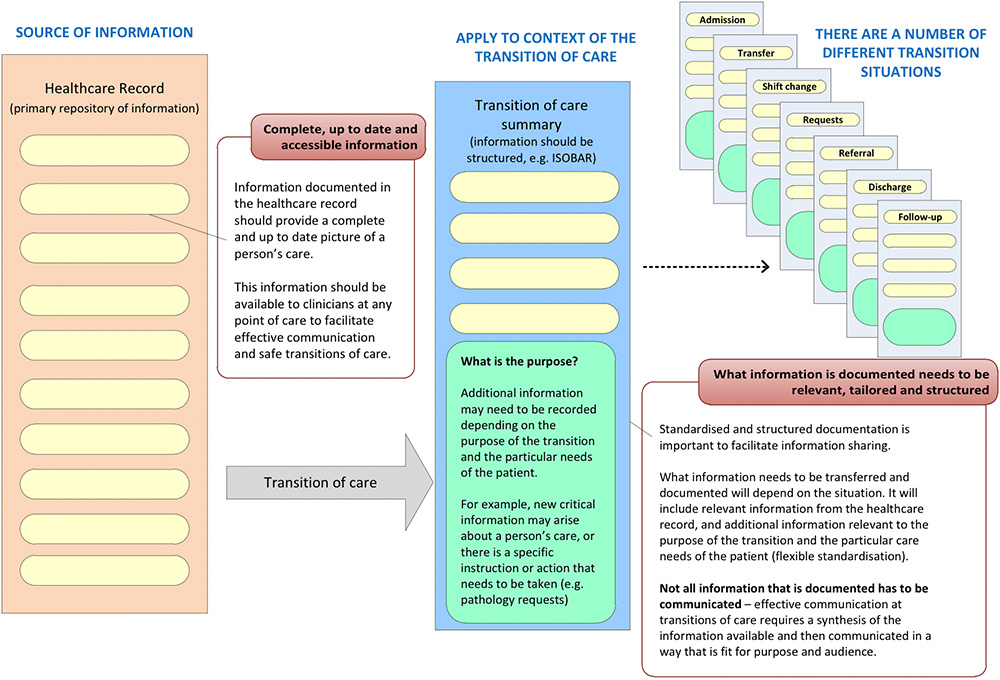
Figure 1 is an example of how the healthcare record is an important source of information for clinicians, and how information available in the healthcare record is used to inform and facilitate safe transitions of care.
How information is transferred, communicated and documented for a transition will depend on the situation and purpose of that transition. Clinicians transferring care will need to exercise clinical judgement and synthesise information to ensure information transferred is fit for purpose, accurate, current and takes into account the specific needs of the patient.
Figure 1: Ensuring information is available to clinicians is essential to facilitate safe and continuous care
Why is it important?
Documentation of information, which is accurate, current, relevant, available and accessible, supports clinicians to deliver safe, high-quality care by ensuring they have correct information to:
- Make safe clinical decisions
- Effectively communicate across transitions with other healthcare providers and across multidisciplinary teams
- Maintain effective continuity of care
- Effectively communicate and partner with patients.
Increasingly, the delivery of health care involves multidisciplinary teams. To ensure safe care, complete and accurate health information needs to be available and shared in a timely way to clinicians responsible for care, and to patients, families and carers. Undocumented or poorly documented information relies on memory and is less likely to be communicated and retained. This lack of communication can lead to a loss of information and result in a number of unplanned or poor outcomes and different types of adverse events.
Evidence shows that poor documentation of information can lead to:
- Higher readmission rates to hospital
- Failure to follow-up after hospital discharge
- Increased costs related to inadequate or reduced care coordination
- Lack of referrals to community service providers
- Increased presentation of emergency departments and increased lengths of hospital stay
- Sub-optimal management of patients’ conditions, inadequate assessment of functional state and inadequate detection of preventable complications in intensive care units
- Lack of availability of important diagnostic results
- Medication errors, including delays and omissions of antibiotics, missed medications and dose errors, and emergency medications being ceased accidently or missed
- Patient deterioration requiring medical emergency team calls and patient falls.
Documentation of information can mitigate some of these safety and quality risks, by ensuring that essential information about a person’s care is available to clinicians, and support effective communication.
Good clinical documentation and high-quality healthcare records also enable clinicians to meet their legal requirements, and for accurate clinical coding to be accomplished.
What does high-quality documentation look like?
Regardless of the medium (paper or digital), high-quality documentation should follow the same guiding principles as outlined in Table 1.
Table 1: Guiding principles for high-quality documentation.
| Guiding principle | What does this look like? |
|---|---|
| Person-centred | Patient’s goals of care are reflected. Information documented is tailored to the specific care needs of the patient, taking into consideration what practical information is needed to support safe care. |
| Compliant | Legislative requirements are met (e.g. privacy and confidentiality) Standards, policies and procedures set by relevant federal, state and territory governments, health services and professional bodies are adhered to, including rules relating to both clinician and patient identification. Standardised language, terminology, symbols and approved abbreviations are used (medications and describing general health terms). Aligned with guidance on structured formats and on-screen presentation. Clinicians provide the right documents and use them in the ways mandated. |
| Complete and accurate | All relevant information is captured (consider any minimum information content requirements). Recorded information correctly reflects the event being documented. |
| Integrated and up to date | Information from all relevant sources is integrated. This includes information from multidisciplinary team members, the patient and their family or carer. Information is up to date (e.g. new or emerging information is recorded, daily progress notes or care plans are documented, and discharge summaries are completed at the time of discharge). |
| Accessible | Documents are available to clinicians who need them, when they need them, and in language that is easily understood by the intended readership. Relevant, up-to-date information is immediately at hand and easy to locate or searchable (physical accessibility). The needs and the capabilities of those who will use the information are considered, and language does not exclude the people who will be using the information. This may include the patient, families, carers and other clinicians across disciplines (deferred accessibility). |
| Readable | Documents are legible and be able to be understood. Whether in electronic or paper, forms and checklists must provide enough space for accurate and legible completion and must include clear instructions about how they should be completed. Acronyms and abbreviations are avoided in both design and completion if there is any potential for ambiguity. Be as specific as possible. |
| Enduring | Documents are materially durable (not loose paper that is likely to be lost or on thermal paper that can fade). The meaning of documents should be maintained, and written to be interpretable by a person who is not present at the time of the recording (self-explanatory). There should be evidence of critical thinking. For example, information should not just simply list tasks but provide enough information and justification to explain recommendations and instructions (actions to be taken and why), and details of the impact and outcome for the particular patient and family involved. |
Specific consideration for patients who are at higher risk
Specific consideration should be given when documenting information for patients with complex and chronic healthcare needs, including:
- Older patients
- Hospitalised children
- People with mental illness
- Patients with multiple comorbidities
- Patients admitted to intensive care
- Aboriginal and Torres Strait Islander patients
- Patients moving along the perioperative pathway
- Palliative care patients.
These patients are a high risk group for patient safety and the complexity and fluidity of information generated for these patients means that documenting up to date, accurate and complete information can be challenging. It is important to consider if there is any additional information that needs to be documented, and ensure that information is tailored to a patient’s specific care needs.
Taking action: What is my role?
Resources
Useful resources that may help you improve documentation of clinical information in your organisation include:
Guides and tools
- Medical records and data-driven healthcare – video (2:29)
- National Guidelines for On-screen Presentation of Discharge Summaries – 58 pages
- Electronic Discharge Summary Systems Self-Evaluation Toolkit – 56 pages
- SHAREing Obstetric Care Clinical handover between VMOs and Midwives – examples of handover documents in obstetric care – Mater Health Services, Brisbane
- Transfer-to-hospital envelope – template for transfers from aged care facility to hospital – North East Valley Division of General Practice
- Yellow Envelope initiative - Brisbane North PHN
- Inter-hospital Patient Transfer Form – based on the ISOBAR structure – Western Australian Country Health Service - 2 pages
- Shared transfer of care templates and tools – TAS Primary Health Network
- Clinical Documents – information about electronic clinical documents – Australian Digital Health Agency
- Recommendations for terminology abbreviations and symbols used in medicines documentation – Summary sheet - 4 pages
- Recommendations for terminology, abbreviations and symbols used in medicines documentation – 16 pages
Further reading
Improving documentation at transitions of care for complex patients -142 pages
A Guide to the Safe Use of Electronic Tools for Clinical Handover - 88 pages