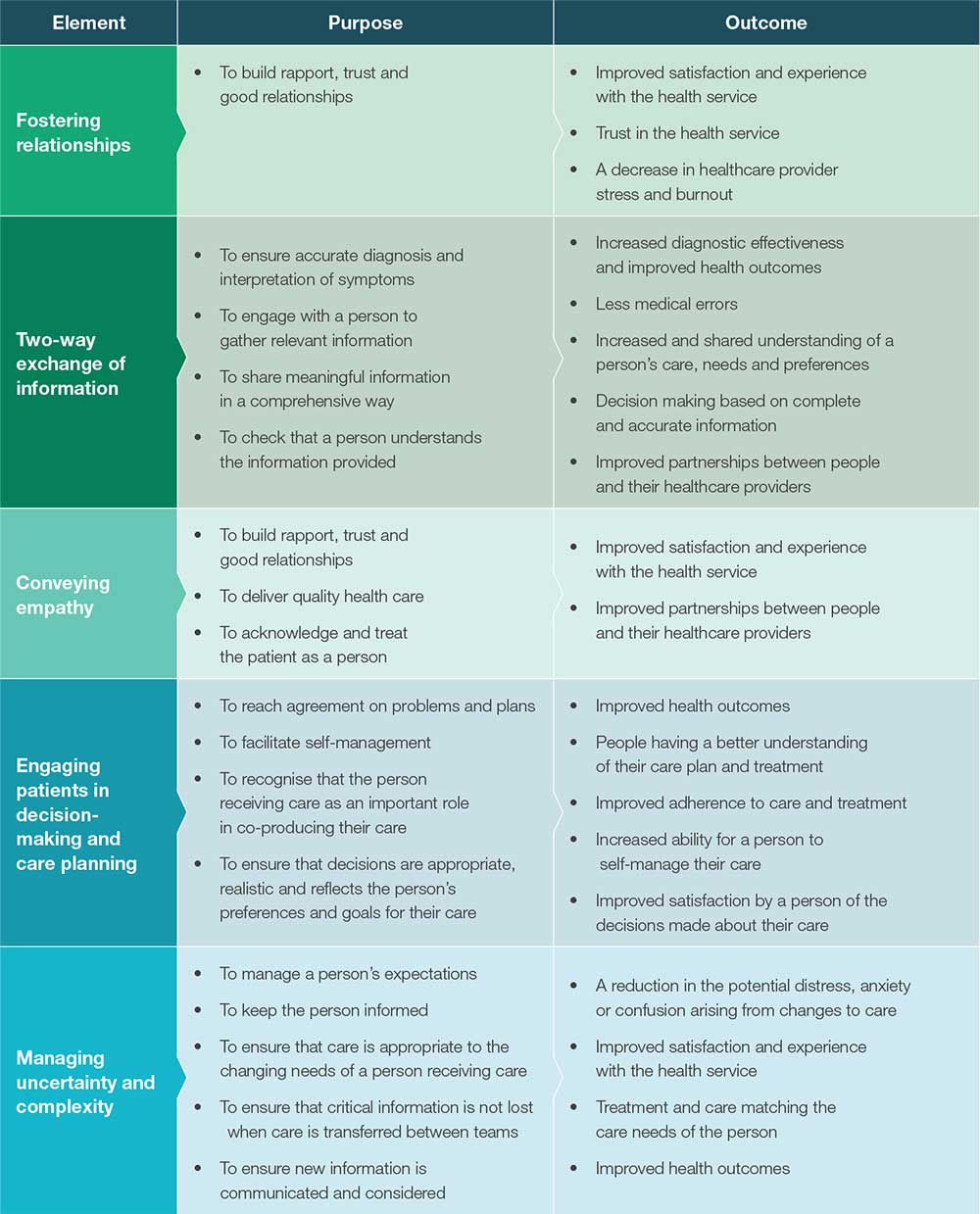
Effective clinical communication is two-way (or multi-way if between teams), structured and continuous communication that results in timely, accurate and appropriate transfer of information. It is tailored, open, honest and respectful, and there is the opportunity for clarification and feedback.
Key messages
What is effective clinical communication?
Clinical communication is the exchange of information about a person’s care that occurs between treating clinicians, members of a multidisciplinary team*, and between clinicians and patients, families and carers.
The process of communication is the way in which information is exchanged. It involves several components – the sender (the person who is communicating the information); the receiver (the person receiving the information); the message (the information that is communicated); and the channel of communication. The way information is delivered, including structure and non-verbal communication (body language, eye-contact and tone) are also important considerations.
Various channels of communication include verbal (face to face, over the phone, via video calls e.g. FaceTime, Skype), written (emails, letters, faxes) and electronic means. Communication processes can occur at the same time, such as verbal communication between two clinicians, or at different times, such as written communication where a clinician documents a patient’s goals, assessments and care plan in the healthcare record, which is later read by another clinician.
*A multidisciplinary team is a team that includes two or more clinicians from multiple disciplines, who work together to deliver comprehensive care. The team may operate under one organisational umbrella or may be from several organisations brought together as a unique team. Multidisciplinary care includes interdisciplinary care.
Why is it important?
Communication failures, lack of teamwork and inadequate documentation in healthcare are known to result in errors, misdiagnosis, inappropriate treatment and poor care outcomes. Evidence shows that:
- Communication problems are a major contributing factor of hospital sentinel events
- Communication failures one of the most commonly cited underlying causes of complaints about the healthcare system.
- Poor medication management and communication can significantly increase the risk of adverse drug events
- Poor communication and transfer of information at discharge can result in an increasing number of readmissions, with lack of effective of communication between health professionals cited as the primary factor that affects post-discharge care transitions
- Poor transfer of information and/or delayed or late referrals can affect quality of care and timeliness of treatment.
Communication skills
Key considerations
Given the complexity of care delivery, the purpose of communication will vary depending on the setting or context of care. To communicate safely there needs to be flexibility and consideration of what is required locally. To determine this it may be helpful to breakdown the communication process into the following key considerations:
| Element | Reflective questions |
|---|---|
WHY are you communicating? |
|
WHO do you need to communicate with? |
|
WHEN do you need to communicate? |
|
WHAT information are you communicating? |
Information should be tailored to the purpose and the person that you are communicating to and about. |
HOW are you communicating? |
|
WHERE are you communicating? |
|
Special considerations for patients at higher-risk of harm
The health workforce needs to be aware that some patient groups can have multifaceted communication issues. This could be related to the complexity of information that can be gathered from the patient, or given to the patient, or complications with language and comprehension, or both. These patients groups may include:
- Aboriginal and Torres Strait Islander people
- Older people
- Disability
- Homelessness
- Cultural and Linguistically Diverse
- Mental Health
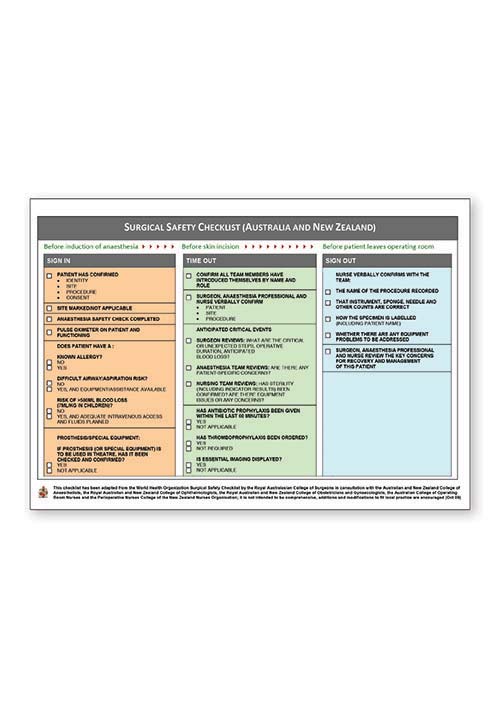
- Undergoing surgery
- Paediatric
- Palliative Care
- Admitted to intensive care
- Multiple co-morbidities.